When I first heard friends getting excited about T-cell immunity to COVID-19, I was non-plussed.
“This means the disease is less contagious than we thought!,” they said.
And I replied, “You’re double-counting! I If some people are immune, that will already be reflected in existing estimates of R0.”
As it turns out, however, my friends were right for the wrong reason. While immunity doesn’t matter for initial estimates of R0, it is crucial for estimating the path of R0. This in turn is crucial for ascertaining when the pandemic will end. David Friedman explains everything with admirable clarity:
Suppose, for simplicity, that half the population consists of people vulnerable to the disease and half, for behavioral or biological reasons, invulnerable. Observing the early spread of the disease, we find that, on average, each infected person passes the disease on to two others. We conclude that we will only reach herd immunity when half the population have had the disease and become immune as a result.
But the relevant figure is not what fraction of the population has become immune but what fraction of the vulnerable population has. In my simple model, half the vulnerable population is only a quarter of the total population, so we reach herd immunity much earlier than the simple calculation implies.
Semi-experts are often quick to say that you can’t reach herd immunity until 60-70% of the population gets infected. If half of the population is immune, however, this is plainly wrong. If 50% of the population is immune, you’ll never hit 60-70% infection rates!
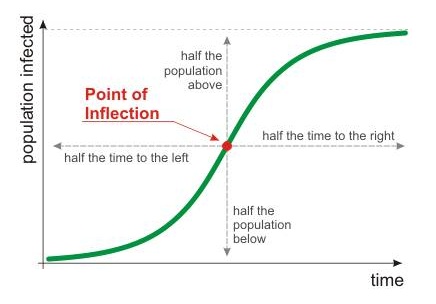
So what’s the correct story? Consider the classic logistic contagion graph:
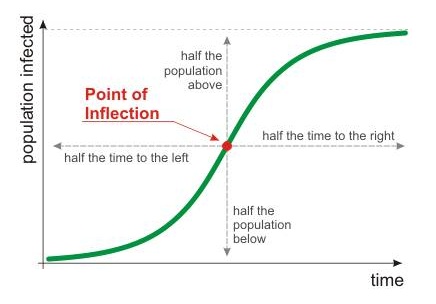
The key question is: Where’s the asymptote for the infected share of the population? If everyone is vulnerable, you probably won’t hit the dashed line until most people get sick. As the immune share of the population goes up up up, though, the dashed line shifts down down down.
The real question, then, is not whether individual immunity helps, but how much. Many countries now look like they’ve hit herd immunity. But as Scott Sumner emphasizes, “herd immunity with the help of drastic behavioral changes” is a far cry from “herd immunity with normal behavior.”
Unfortunately, both versions of herd immunity superficially look the same. To tell them apart, you have to relax behavior and restrictions and see if the pandemic returns. So while my improved understanding of the mathematics of immunity makes me more hopeful in the long-run, in the medium-run I remain diffident. I won’t be surprised if the pandemic is over in every U.S. state by Christmas. I won’t be surprised if the pandemic is worse in every U.S. state by Christmas.
Closing thought: The extreme rarity of public bets on the path of the pandemic tells me that even the best-informed experts remain about as confused as I am. They’re just too high on their own punditry to admit that they know little indeed about what’s going to happen. I wish they would read Tetlock’s Superforecasting before they speak another overconfident word, but I know they won’t.

READER COMMENTS
William Kiely
Sep 2 2020 at 11:41am
I might be willing to bet against you here depending on what exactly you mean.
By “I won’t be surprised” do you mean that your credence each outcome will occur is >X%? If so, what is the X% you have in mind that you’d be willing to bet on?
Warren Platts
Sep 2 2020 at 12:09pm
I would say the pandemic is basically over in Sweden, where the number of daily deaths is < 10. Since USA has 30X more people, we can define the end of the pandemic when average daily deaths get below 300.
Assuming no heroic measures (and the ones we have are largely being ignored), and simply extrapolating the decline in deaths, we should get to below 300 deaths/day by the middle of November, so end of pandemic by Christmas is a fairly safe bet. Probably get below 10/deaths per day by end of February.
Warren Platts
Sep 2 2020 at 11:45am
Respectfully beg to differ. The closest western country with normal behavior was Sweden. There was a big 1st wave, and then a gradual decline with no second wave. Now the number of daily deaths are less than 10. It looks like they have achieved herd immunity, pretty much.
Meanwhile, places that managed to curb deaths through lockdowns are predicted and observed to experience 2nd waves once the lockdowns are relaxed.
Jose Pablo
Sep 2 2020 at 2:27pm
“Sweden has reached” herd immunity is a curious claim.
According to the data there have been 85,000 Covid cases in Sweden. With a population of, roughly, 10 million, it means 0.85% of the population affected by the virus.
Serology studies suggest around 10% of the population has been infected (which means 90%+ cases go undetected !!). Only one serology study, out of 3, among Sweden health workers at a single hospital, reports 20% of seropositive.
Claiming that Sweden has reached herd immunity is equivalent to claim that herd immunity can be reached with around 15% of the population infected.
DeservingPorcupine
Sep 2 2020 at 2:35pm
But we know for a fact now that serology studies undercount unless you test everyone right during or just after infection. Antibodies from mild or asymptomatic cases disappear quickly, leaving T cell/B cell-mediated resistance. That’s why antibody prevalence in NYC and London are going down over time.
Jose Pablo
Sep 2 2020 at 3:31pm
Maybe, but in the Swedish case, the undercount has to be “very” severed (65-75% of the infected not been detected) to move the 15% of people affected to the 50-60% normally claimed as required for herd immunity.
If this is your claim, that is equivalent to say that serology studies are useless and leaves us without any valid way of knowing how many people has been affected in an area.
If the “undercount” is closer to something like 2 in 3 cases detected, still claiming that Sweden has reached herd immunity is equivalent to claim that it could be reached with around 20-25% of the population affected. Much lower than normally claimed.
DeservingPorcupine
Sep 2 2020 at 7:10pm
Yes, serology studies are useless for broad populations where there are many mild cases and where people were exposed at different times. Not sure why broad T cell testing hasn’t been undertaken. I’m guessing it’s relatively expensive.
And yes, it’s clear that effective herd immunity is achieved at a level much lower than the typical ~60% for reasons that have been often discussed. Heterogeneous susceptibility, large pools of pre-existing immunity due to other coronavirus exposure, etc.
Warren Platts
Sep 2 2020 at 5:25pm
Yes. That is not too far from what I’m saying. This guy, Karl Friston, a famous statistician, predicts that when all is said and done, Sweden’s susceptible population will turn out to have been around 20%..
https://unherd.com/2020/06/karl-friston-up-to-80-not-even-susceptible-to-covid-19/
DeservingPorcupine
Sep 2 2020 at 11:54am
I would happily make a bet on whether or not the pandemic will be worse by December in a number of states. What odds would you require for this bet?
The seven-day average of new covid cases in Florida will not exceed its current peak value of 11,943 from July 17th.
I’d be willing to take heavily-tilted odds, like 1:20.
robc
Sep 2 2020 at 7:52pm
I would probably give 100:1 on NY state.
Josh
Sep 2 2020 at 12:00pm
But R is also proportional to the remaining number of susceptible people, so in areas with significant infections, R is naturally lower even without social distancing
Eg if half the people were immune to start then the initial R0 was actually more like 5, not 2.5. If now we find that 20% of the people have been infected as in hard hit places like the northeast US, then that means only 30% remain susceptible. So R is now 5*0.3 = 1.5, which is only slightly worse than the flu.
And then when just 5% more get infected, the R is down to 1.25 which is slightly slower than the flu. Etc.
So going forward in many places, even with no social distancing, we’ve got a virus that spreads with roughly the same speed as the flu, which we know how to deal with. And keep in mind, the problem in places like NYC wasn’t how bad the disease was, it was how fast it spread. Something like 2m New Yorkers got infected in a couple months, which is what strained the hospitals. That fast spread simply can’t happen again any place that had a significant first wave, with or without social distancing.
Steve
Sep 2 2020 at 1:49pm
What bets would you be willing to make given all of your knowledge up to this point?
I would not be willing to bet on an absolute magnitude of the number of COVID deaths by the end of 2020, but I would be willing to bet on a given rate of deaths. Say…total deaths from 9/1-12/31 will be less than total deaths from 5/1-8/31? Or even: deaths/confirmed cases will be lower in month of December than in month of September. But maybe that’s not too controversial of an opinion to have anyone take the other side?
Jose Pablo
Sep 2 2020 at 3:17pm
I am still puzzled by the lack of granularity in the “thoughts” regarding this virus.
“Transmission rates are irrelevant”. With a very significant number of cases (close to 80 or even 90% according to some analysis) going undetected, getting or not the virus (which is what “transmission rates” are all about) is meaningless. “Hospitalization rates” (or even death rates) are a much more relevant metric. Sure, they depend on transmission rates, but also on a lot of other variables that, once properly understood, could be acted upon limiting the “true impact” of the virus (which, apparently, is not only related with “getting the virus”)
“Global data are irrelevant”. Despite their global reach this is a very “local” virus. 1.- The relevant transmission rates are local. Sure, the transmission can be sparked by an imported case, but, still, how this “case 0” affects a community depends on local transmission mechanisms. 2.- The impact on the health system is local 3.- The “susceptibility” of the populations to relevant consecuences in an area depends on very local characteristics (average age, preexisting conditions prevalence, …)
Based on that:
Why don´t we have “Susceptibility Indexes” at a county (or even city) level? Measuring the probability of the virus sending people to a hospital (or killing them) in that area. I am pretty sure the dispersion of this “local indexes” is going to be startling.
Why don´t we have analysis of a “hospitalization R” (meaning how many people get hospitalized for every person that get discharged) or even “death R” (how many people die for every person death)?. It is just a feeling but for this virus (with such a huge dispersion in the severity of the symptoms) understanding the differences between “transmission rates” and these “hospitalization/death transmission rates” could point us to drivers of the severity of the illness that could be acted upon (remember, the “severity” and not the “transmission” is the relevant concept … and they seem to be very different)
Why haven´t we developed “personal susceptibility indexes” (based on age, general health status, …) that allow us to better understand the risk we, as individulas, face in our very local day to day live in the middle of this “not so global” pandemic?
A Country Farmer
Sep 2 2020 at 9:23pm
Early on, I bet my friend $100 that total U.S. deaths would be below 100K. I was wrong and learned a painful lesson of being too blasé about things!
Comments are closed.